Preparing for Breast Cancer Surgery
There are some important steps to get ready for this procedure.
A detailed medical history where information is provided to the medical team on any medications, including vitamins and supplements. Previous allergies or reactions to medications or surgical procedures in the past is documented.
Preexisting conditions can affect how the body responds to surgery, such as heart disease, diabetes, or high blood pressure. It is important for the team, including the anaesthetist to know this.
Blood transfusion is rarely required, but may be organised in case it becomes necessary.
As the date approaches, a series of tests are done for you including a Chest X-ray, ECG, and blood tests.These tests let your doctor know if your body is ready for the operation.
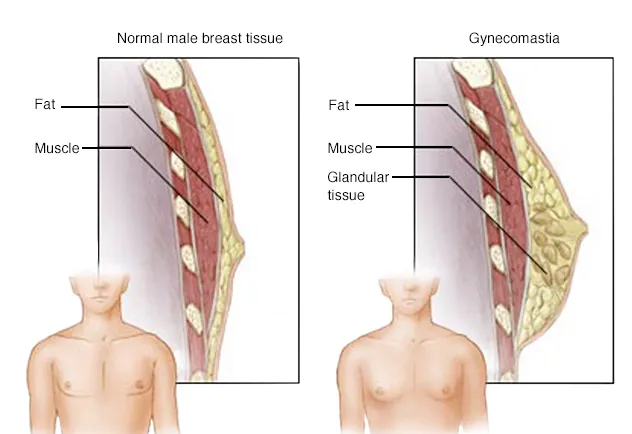
Specific tests depending on your procedure may be needed, a CT scan to check the size and location of your tumour. Lymphoscintigraphy for sentinel node biopsy.
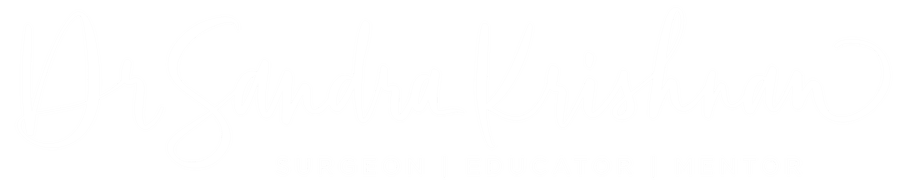
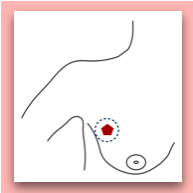
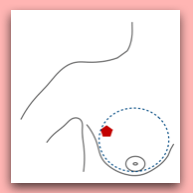
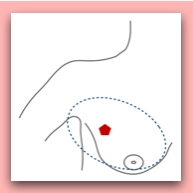
Preoperative localisation procedure may be required, if the tumour is not felt, this may involve ultrasound and/or mammography and a hook wire in most centres.
How to deal with pain after Breast Cancer Surgery?
This procedure is remarkably painless for the most part, partly due to operating in existing planes and not cutting any muscle. The intensity and duration of post operative pain depends on extent of the procedure and whether a oran has been used. Intravenous or oral analgesics will be provided to keep as comfortable as possible. Gentle exercises to start mobilising, gradually increasing activities as the days go by, with adequate pain relief is recommended.
What is Breast Cancer Surgery recovery time?
The length of your stay in the hospital is variable. It depends on the type of procedure being done, how the body tolerates the operation which is dependent on the above and general health.
Lumpectomies can be day procedures. The recovery takes place in the day surgery centre and you will likely go home later the same day if everything is routine.
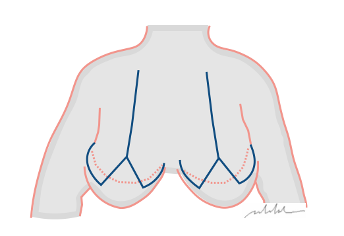
If you have a mastectomy or an axillary lymph node dissection, you will probably stay in the hospital for 1 or 2 nights.
What to expect after Breast Cancer Surgery?
A breast care nurse will be helping you along the journey, from before surgery to after care. You will be given information on wound care, exercises and return to daily activities, and a post operative appointment for a wound review and discussion of the pathology. This is when the most information becomes available, and a comprehensive treatment plan will be discussed.
Long term recovery from surgery is 100%. Donald McKenzie, a Canadian sports medicine specialist in February 1996 he started a dragon boat team for women with a history of breast cancer, which the women chose to name Abreast in a Boat. His paper concludes: ‘promoting health and raising breast cancer awareness that is driven by women with the disease. It reaches out to other women and offers them a message of hope and support. It is helping to change attitudes toward "life after breast cancer," and it encourages women to lead full and active lives. It is making a difference.’